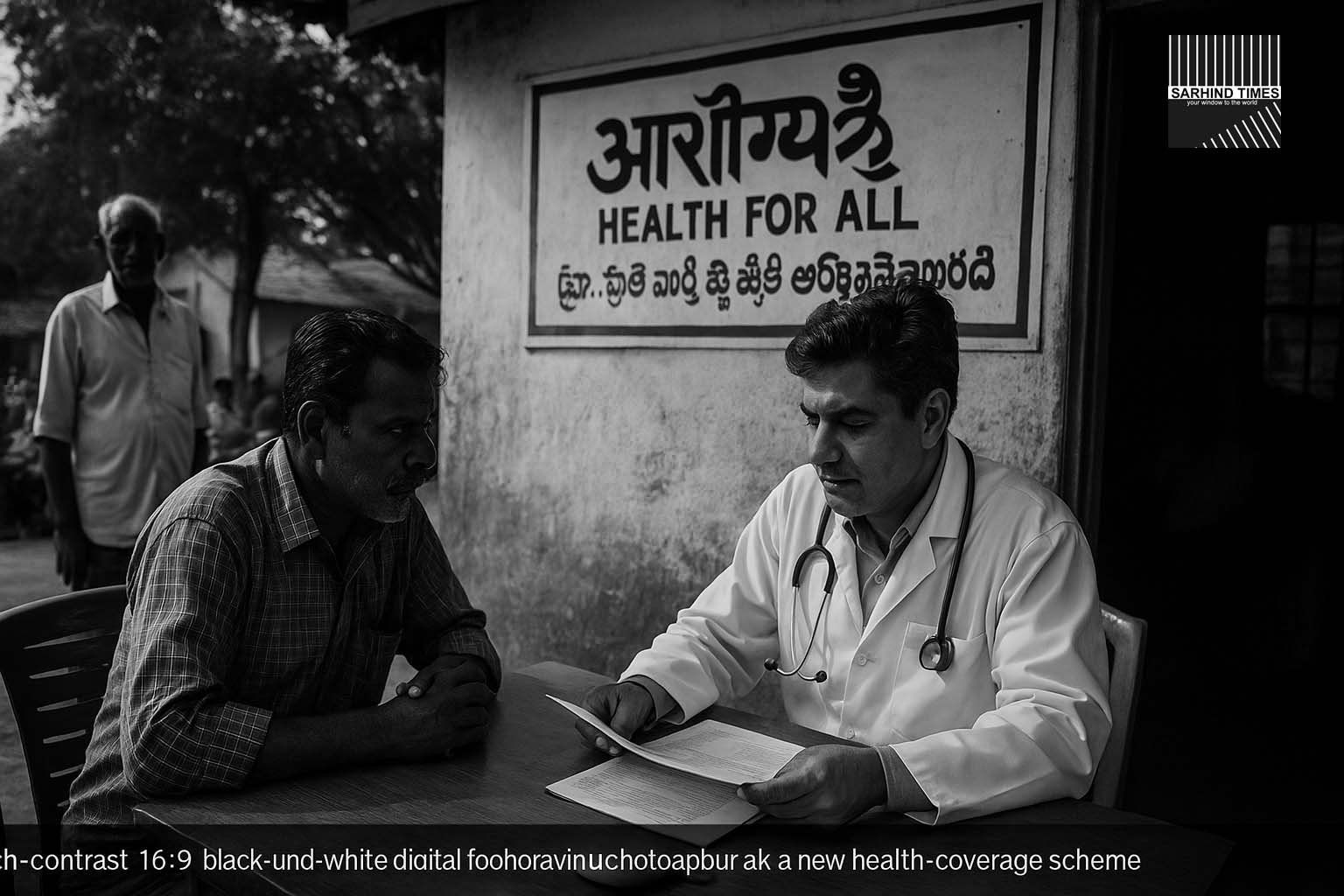
State government unveils “Sanjeevani Project” to expand health assurance with up to ₹25 Lakh support for the poor and digitise 6 crore medical records
Dateline: Guntur | 11 November 2025, Asia/Kolkata
Summary: The government of Andhra Pradesh has announced a sweeping universal health‐coverage scheme under which every resident will receive health-insurance cover of up to ₹2.5 lakh per family. For poor households, additional benefits up to ₹25 lakh have been specified. Branded under the “Sanjeevani Project”, the scheme also aims to digitise medical records of approximately 6 crore residents and forge cutting‐edge partnerships for care delivery. Analysts say this is among the most ambitious state-level health assurances in India, signalling a major step in affordable access—but execution may face fiscal, logistical and structural challenges.
Context and Rationale
In announcing the new health-insurance initiative, Chief Minister N. Chandrababu Naidu stated that the scheme aims to fulfil accessible and quality healthcare for all residents of Andhra Pradesh, irrespective of income, location or age. The state currently faces a dual challenge of rising out-of-pocket spending for health, and disparities in access between urban and rural areas. The new scheme attempts to reduce the burden of catastrophic health expenditure, improve preventive and curative infrastructure, and strengthen the digital backbone of health services.
According to government briefings, the scheme will provide each resident a basic cover of ₹2.5 lakh annually (or per family unit, subject to final design) and eligible vulnerable households will receive enhanced medical support up to ₹25 lakh. The “Sanjeevani Project” also plans large-scale digitisation of medical records, starting with the 6 crore population of the state, and partnerships with both domestic and international institutions (including foundations) for knowledge and technology transfer.
The healthcare financing gap in Andhra Pradesh—particularly among rural households and lower-income urban residents—has been a concern. The state estimates that nearly 8–10 % of its population incurred major healthcare expenses annually; high costs have led to delayed treatment, medical impoverishment and limited preventive care uptake. Through this scheme, the government aims to reduce financial barriers, improve preventive health access, and build system capacity for diagnostics, tertiary care and follow-up.
Scheme Features and Implementation Pathways
Key structural features of the scheme include:
– **Universal coverage design**: The scheme is designed to cover all residents of the state—no means-testing required for the base ₹2.5 lakh cover.
– **Enhanced benefit lane**: Poor or vulnerable households (criteria to be finalised) will access limits up to ₹25 lakh covering serious illnesses, tertiary care, transplants, long-duration hospitalisations.
– **Digitised medical records**: A major component of Sanjeevani is creation of unified digital health-records system for all 6 crore residents, enabling portability, diagnostics linkage, and analytics.
– **Public-private partnerships**: The state will invite bids/partnerships with private health-care networks, international foundations (including mention of the Bill & Melinda Gates Foundation in the announcement) and technology firms to boost service capacity and infrastructure.
– **Outreach and preventive care**: Alongside hospitalisation cover, the scheme emphasises screening, diagnostics, early-intervention programmes and community health centres, to reduce demand shock on tertiary care.
– **Budgetary & funding design**: Officials indicated that the state budget will allocate initial seed-funding for FY 2025-26 and restructure the existing health-insurance programme to integrate with the new universal cover. The expectation is that improved preventive care and early treatment will over time reduce cost escalation.
Implementation will follow phases: pilot roll-out in selected districts before full state-wide launch, contracting hospitals and network providers, finalising beneficiary registries and setting up digital architecture.
Expected Benefits and Access Impacts
If successfully implemented, the scheme could deliver multiple benefits:
– **Reduced out-of-pocket expenditure** for middle- and lower-income households who currently bear the brunt of medical costs.
– **Increased service utilisation** particularly in rural and remote districts where tertiary care options are limited; addressing access gaps may improve health outcomes (maternal mortality, NCD management, transplant access).
– **Digitising health-records** can lead to continuity of care, better referral systems, data-driven policy interventions and improved care-quality monitoring.
– **Stimulus for private health-care investment**: With large-scale insurance cover and predictable beneficiary base, private hospitals and diagnostic chains may expand more rapidly, improving infrastructure availability and competition.
– **Economic uplift**: Health-secure populations translate into stronger workforce productivity, lower vulnerability to medical shocks, and potential attraction of health-care and associated service industries to the state.
For service providers and content/automation firms, the scheme opens demand contexts: digital health-records implementation, voice/AI modules for beneficiary awareness, multilingual outreach, claims-processing automation, hospital-network workflows, and data-analytics platforms for preventive-care metrics.
Challenges and Risks Ahead
Notwithstanding the promise, several structural risks remain:
– **Fiscal burden**: Universal health coverage, especially with high-end benefits, imposes significant cost; sustainability over multiple years will require cost-control, premium design, supplier management and demand-modulation.
– **Provider capacity**: The state must ensure availability of tertiary hospitals, specialist doctors, transplant centres and diagnostics. Rural service gaps, referral delays and infrastructure deficits may bottleneck access.
– **Digital infrastructure**: Digitisation of 6 crore health records is complex—data-privacy, interoperability, beneficiary authentication, citizen digital-literacy and infrastructure readiness are major hurdles.
– **Fraud and misuse risk**: Large insurance-rollouts are vulnerable to abuse (over-billing, ghost patients, improper claims). Robust governance, audit, digital-verification and automation are essential.
– **Behavioural and preventive-care alignment**: Unless preventive and primary-care systems are strengthened, increased cover may lead to overuse, cost inflation, and load on tertiary services—not necessarily improved outcomes.
– **Transition risk**: Integrating legacy schemes, managing network provider contracts, training workforce, and aligning multiple departments is administratively heavy—delays could dent public trust.
For your sector (content + automation), these challenges mean you may find early demand in pilot districts, but must structure services that emphasise governance, audits, workflows and capacity building rather than just benefit-advertising.
Strategic Implications for Andhra Pradesh and Beyond
The scheme positions Andhra Pradesh at the forefront of state-level health-policy innovation. Key implications:
– **Competitive state advantage**: As health-access improves, Andhra may attract healthcare investment, medical-tourism flows, specialised services and corporate campuses preferring regions with strong health safety nets.
– **Digital health ecosystem growth**: Creation of unified records system enables downstream services—analytics, remote monitoring, tele-health, AI-based diagnostics—that will open service-provider opportunities, including multilinguistic and voice/AI workflows.
– **Manufacturing and device ecosystem**: Increased utilisation of diagnostics and care may drive demand for medical devices, digital-health tools and health start-ups, furthering the state’s manufacturing and innovation advantage.
– **Policy-model for others**: If successful, the Andhra scheme may serve as a template for other states, spurring competitive health reforms and service-provider demand across India.
For your business (content/automation) this means you may target not just Andhra but other states preparing to upgrade health-digital ecosystems. Creating reusable modules, multilingual content, automation templates for health-insurance workflows, tele-health onboarding processes, and compliance modules will give you early positioning.
What to Watch in Coming Months
Key signals to monitor include:
– The official launch date and roll-out schedule (district-wise) of the scheme.
– Details of beneficiary registration process, eligibility criteria, hospital network empanelment and claim-processing workflows.
– Government tender notices for digital-records implementation, claims-processing software, tele-health platforms, and training of health-workers.
– Private-sector partnership announcements (hospital chains, diagnostics firms, technology platforms) and investment commitments in Andhra’s health-care ecosystem.
– Data on utilisation: number of dossiers registered, number of claims filed, outpatient and inpatient service shifts, cost and premium analytics.
Early mover service-providers should position pilots aligned to the scheme’s modules (registration, claims, reporting, vernacular outreach). Multi-language voice-content (Telugu, English, Hindi) will likely be required.
Conclusion
The announcement of a universal health-coverage scheme in Andhra Pradesh marks an ambitious leap in state-level healthcare reform. The blend of broad insurance cover, enhanced benefits for the poor, and a strong digital-health component sets the stage for transformative impact—if executed well. For residents it promises relief; for industry and service-providers it opens new frontiers of opportunity; for policy-observers it signals a shift in public-health governance.
But ambition is only half the story. The delivery will require fiscal discipline, infrastructure scale-up, digital implementation and risk management. The next months will determine whether the scheme becomes a durable model for universal care, or a policy headline with limited traction.
For your work in content creation, automation and voice/AI services, this is a moment to move from observation to action: build service modules, create pilot scripts, develop multilingual outreach content and engage with early-stage health-partners or start-ups. The window is open — how you respond will shape whether you capture the opportunity.



+ There are no comments
Add yours